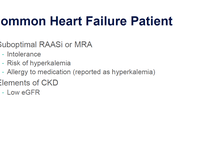
Patients with heart failure and chronic kidney disease (CKD) are challenging to manage. The best approach is a multidisciplinary one, which will help to optimize guideline-directed medical therapy in patients at risk for hyperkalemia. Join Drs. Ellie Kelepouris and Stephen Greene as they discuss how to identify patients at high risk of developing hyperkalemia and the available treatment strategies for these complex patients.
Disclosure of Conflicts of Interest
In accordance with the ACCME Standards for Integrity and Independence, Global Learning Collaborative (GLC) requires that individuals in a position to control the content of an educational activity disclose all relevant financial relationships with any ineligible company. GLC mitigates all conflicts of interest to ensure independence, objectivity, balance, and scientific rigor in all its educational programs.
Host:
Ellie Kelepouris, MD, FACP, FAHA
Professor of Clinical Medicine
Perelman School of Medicine
Hospital of the University of Pennsylvania
Philadelphia, PAConsulting Fees: AstraZeneca, Bayer, Boehringer Ingelheim/Lilly, CSL Vifor
Faculty:
Stephen J. Greene, MD, FACC, FHFSA
Heart Failure Cardiologist
Duke Clinical Research Institute and Duke University School of Medical
Durham, NCConsulting Fees: AstraZeneca, Bayer, Boehringer Ingelheim/Lilly, Bristol Myers Squibb, Corteria, Cytokinetics, CSL Vifor, Lexicon, Merck, PharmaIN, Roche, Sanofi, Tricog, Urovant
Contracted Research: AstraZeneca, Boehringer Ingelheim, Bristol Myser Squibb, Cytokinetics, Merck, Novartis, Pfizer, Sanofi, PfizerReviewers/Content Planners/Authors:
- Megan Clem has nothing to disclose.
- Cindy Davidson has nothing to disclose.
- Ann Early has nothing to disclose.
- Amanda Hilferty has nothing to disclose.
- Brian P. McDonough, MD, FAAFP, has nothing to disclose.
- Tim Person has nothing to disclose.
- Mario P. Trucillo, PhD, MS, has nothing to disclose.
Learning Objectives
After participating in this educational activity, participants should be better able to:
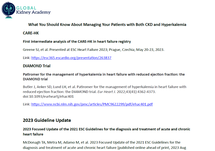
- Explain the therapeutic rationale of using potassium binders to manage hyperkalemia in the short and long term to improve outcomes in patients with chronic kidney disease (CKD) who are on RAASi therapy
- Identify multidisciplinary medical management strategies for challenging patients with multiple comorbidities
- Differentiate the risks and benefits of currently available potassium binders based on recent clinical trials in patients with CKD
Target Audience
This activity is designed to meet the educational needs of nephrologists, endocrinologists, primary care physicians, cardiologists, and all HCPs involved in the identification and treatment of HK in CKD patients.
Accreditation and Credit Designation Statements
 In support of improving patient care, Global Learning Collaborative (GLC) is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC) to provide continuing education for the healthcare team.
In support of improving patient care, Global Learning Collaborative (GLC) is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC) to provide continuing education for the healthcare team.The American Medical Association has an agreement of mutual recognition of Continuing Medical Education (CME) credits with the European Union of Medical Specialists (UEMS), the accreditation body for European countries. Physicians interested in converting AMA PRA Category 1 CreditsTM to UEMS-European Accreditation Council for Continuing Medical Education CME credits (ECMECs) should contact the UEMS at mutualrecognition@uems.eu.
Global Learning Collaborative (GLC) designates this enduring activity for a maximum of 0.25 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Global Learning Collaborative (GLC) designates this activity for 0.25 nursing contact hours. Nurses should claim only the credit commensurate with the extent of their participation in the activity.
Provider(s)/Educational Partner(s)

Our ultimate goal is to improve the care being delivered to patients, and our high-quality, evidence-based CME initiatives reflect our dedication to the creation and execution of excellence and are the product of shared research, knowledge, and clinical practice skills across the healthcare continuum.
Commercial Support
This activity is supported by an independent educational grant from CSL Vifor.
Disclaimer
The views and opinions expressed in this educational activity are those of the faculty and do not necessarily represent the views of GLC and Medtelligence. This presentation is not intended to define an exclusive course of patient management; the participant should use his/her clinical judgment, knowledge, experience, and diagnostic skills in applying or adopting for professional use any of the information provided herein. Any procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this activity should not be used by clinicians without evaluation of their patients’ conditions and possible contraindications or dangers in use, review of any applicable manufacturer’s product information, and comparison with recommendations of other authorities. Links to other sites may be provided as additional sources of information. Once you elect to access a site outside of Medtelligence you are subject to the terms and conditions of use, including copyright and licensing restriction, of that site.
Reproduction Prohibited
Reproduction of this material is not permitted without written permission from the copyright owner.System Requirements
- Supported Browsers (2 most recent versions):
- Google Chrome for Windows, Mac OS, iOS, and Android
- Apple Safari for Mac OS and iOS
- Mozilla Firefox for Windows, Mac OS, iOS, and Android
- Microsoft Edge for Windows
- Recommended Internet Speed: 5Mbps+
Publication Dates
Release Date:
Expiration Date:











Facebook Comments