We now have evidence-based options to reduce atherosclerotic cardiovascular disease (ASCVD) event burden beyond any previously available therapy. A collaborative approach to addressing residual cardiovascular risk across a variety of risk factors that goes beyond LDL-C-lowering therapies is needed to optimally manage patients with or at high risk of ASCVD. Pharmacists treating these patients will benefit from a review of recent data and guidelines so they can incorporate these findings into clinical practice. Join us to ensure you’re keeping up with the science and giving your patients the best care.
Addressing Patient Management in ASCVD Risk Reduction: A Collaborative Approach
Addressing Patient Management in ASCVD Risk Reduction: A Collaborative Approach
Addressing Patient Management in ASCVD Risk Reduction: A Collaborative Approach
Announcer:
Welcome to CME on ReachMD. This activity, titled Addressing Patient Management in ASCVD Risk Reduction: A Collaborative Approach is provided by Medtelligence and is supported by an independent educational grant from Amarin Pharma, Inc.
This replay of a live broadcast discusses a collaborative approach to reducing ASCVD event burden in your high-risk statin-treated patients.
Dr. Cheeley:
We as pharmacists play such an important role in today’s managed care environment. Having an informed dialogue with prescribing physicians is crucial when using a collaborative approach to manage these sometimes difficult-to-treat patients.
Welcome to this AMCP [Academy of Managed Care Pharmacy] eLearning Days virtual satellite symposium. I’m joined by Dr. Chuck Vega who is a primary care physician. We’re going to break down the differential biological effects of omega-3 fatty acids and the clinical implications of major clinical trials. We’ll also cover practical considerations in using IPE [icosapent ethyl] in ASCVD [atherosclerotic cardiovascular disease] management and define the shortfalls of dietary supplements.
Today our learning objectives include: to outline the biological effects of omega-3 fatty acids and their mechanism of action, differentiating icosapent ethyl from other agents. We’re going to talk about engaging with our physician partners to interpret and relate recent clinical trial evidence of EPA [eicosapentaenoic acid] and the clinical implications to patients. And lastly, we’re going to distinguish the use of icosapent ethyl, or IPE, in ASCVD management and define the shortfalls of dietary supplements.
This is CME on ReachMD, and I’m Dr. Mary Katherine Cheeley.
Dr. Vega:
And I’m Dr. Chuck Vega.
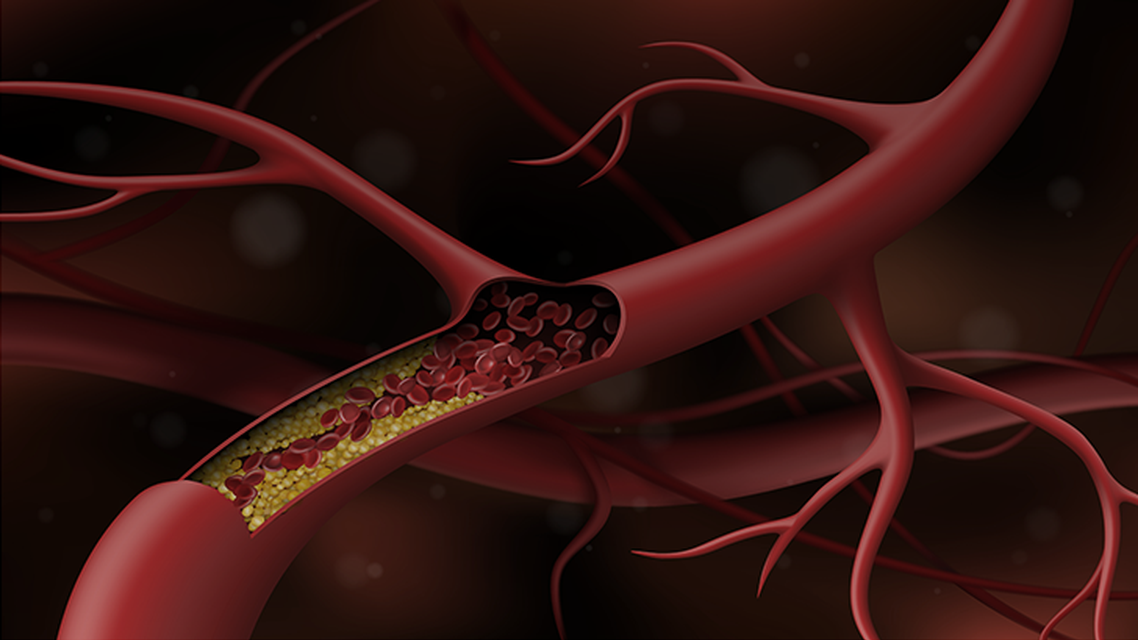
So let’s start with just a short review of the burden of heart disease overall. And so just as a level-set for everybody, when we think about major adverse cardiovascular events [MACE] or cardiovascular disease, of course we have to think about coronary heart disease among first and foremost in the form of either MI [myocardial infarction] or unstable angina or folks who’ve had a revascularization procedure. You can see those listed here. But we also have to think about stroke or TIA [transient ischemic attack], carotid artery stenosis, peripheral artery disease, and renal artery stenosis certainly goes with a lot of the same risk factors we see with cardiovascular disease. And it’s something that is under recognized in clinical practice as well.
And heart disease, every talk that we give is required by law that we mention COVID-19, and so this one is no different. So we did see an increase in the rate of cardiovascular death overall during the pandemic and of course, cardiovascular disease always has been the number one killer of US adults for decades. While we see a rising prevalence of cardiovascular events among women, it’s still more common among men, and you can see the difference in rates of mortality and percentage of mortality overall.
So this is something that we see in our clinical practices every day. The key is to mitigate risk factors so we can prevent major cardiovascular events, such as revascularization, or worse, a heart attack or a stroke.
And as we said, statins are used all the time in my practice, as well, I’m sure, as in yours, so they are foundational because they work. We have many great randomized trials that show that statins are effective both in primary and secondary prevention against cardiovascular disease. But you can see from this graphic that they are not the be-all and end-all when it comes to prevention of cardiovascular events. In fact, there is a substantial risk no matter which statin you’re using. Whether you’re talking about a low-intensity statin or a high-intensity statin, there remains a lot of cardiovascular risk that’s left over and left on the table, and unfortunately, folks with more cardiovascular risk factors, even though they are taking the appropriate statin, many still go on to have heart attacks, strokes, and revascularization.
And one question that comes up frequently is, gosh, could I push the LDL level too low? It doesn’t seem like there really is a bottom point. You might get a little bit less impact as you go to very low levels of LDL cholesterol, say, less than 50 mg/dL, but certainly, there doesn’t seem to be any harm in doing so, and for certain patients with multiple risk factors and a prior history of cardiovascular disease, you really want to get them lower because you can see in this study that was looking at a PCSK9 inhibitor and LDL-C values, in 3-year event rates, you can see that the lower you go, generally the better the event rates are. The more high risk the patient is, the more effects you’re going to have in terms of lowering LDL cholesterol. You’ll have a greater overall impact on the risk of cardiovascular disease because their risk in the first place was fairly elevated.
And this is one of my more favorite slides in this section because it’s looking at cardiovascular risk from a more holistic perspective. Absolutely, LDL cholesterol is part of it, but look at these other important factors. We know that inflammation and diabetes and having a thrombogenic state, all of those things, along with triglycerides and lipoprotein(a), which are major cardiovascular risk factors in and of themselves – and we’re going to delve into that – they all need to be addressed. And I think this is something that I do fairly well in my practice. Of course, I’m going to push on LDL, and I’m going to use a statin to its full extent based on the patient’s profile, but I’m not going to lose sight of the fact that I have to manage not only their triglycerides and their diabetes, but also their obesity and their blood pressure as well. And sometimes, yeah, we know that we can’t necessarily push all of those factors down. Some patients may respond more to LDL lowering with a statin. Some patients may be more amenable to, okay, well, I don’t really want to take these specific 3 drugs for my diabetes, but I will take 2 drugs for my hypertension. Of course, we’re going to go, because all of that is to the good; all of it helps reduce that cardiovascular risk over time.
So I just want to make a shout-out to a pragmatic approach and a holistic approach to cardiovascular risk reduction. It starts for most of my adults with using the American College of Cardiology [ACC]/American Heart Association [AHA] risk calculator. I’m sure many of you are familiar with the risk calculator, and you probably know that it’s not perfect for those adults ages 40 to 79 years of age. It does give you a 10-year cardiovascular risk, and it comes with recommendations for particularly how to use statins and perhaps aspirin as well. The calculator is not perfect, I always like to say, but it does put you in the ballpark, and it gives you an objective measure for assessing cardiovascular risk.
Now let’s switch a little bit and think about triglycerides specifically. Triglycerides don’t have the body of research, particularly in terms of treatment, that, say, LDL cholesterol dose, but they still are very important as a potential risk factor for cardiovascular events. And we are not talking about triglycerides, you know, in the 300 mg/dL range. You can see that, through this graph – and this is research that was done in the Atherosclerosis Risk in Community study – that even a moderate increase in triglycerides is associated with a higher risk of cardiovascular disease. So this is something we have to be continuously monitoring patients for. So I think we did ourselves a great disservice, oh, 10 to 15 years ago when it was, well, let’s just start a statin, and then you really don’t have to worry about cholesterol anymore because, frankly, you’ve started the statin; you’re doing everything you can do. And that is not the way to think about it because we can miss important factors. Even if the LDL is controlled, and even if they have cardiovascular disease, if their triglycerides are elevated, we have to consider that as another potential cardiovascular risk as well.
These are important things to consider, and they’ve come out in guidelines regarding the management of triglycerides. So particularly and among individuals with elevated triglycerides, and that could be just a fasting triglyceride level of 150 mg/dL or more, and particularly when they have either a history of cardiovascular disease or they have diabetes, so we’re going to initiate by thinking about lifestyle factors. So we are going to look at diet, and we are going to look at exercise. We’re going to think about concomitant conditions that can promote hypertriglyceridemia. We are very importantly going to look at medications which could promote hypertriglyceridemia because we don’t want to iatrogenically increase patients’ cardiovascular risk.
Next step, we are going to be looking at statin therapy. Statin therapy because patients with diabetes and established cardiovascular disease, statin therapy, again, foundational. “Why are you not on a high-intensity statin?” is usually my question. If they’re not, then I really have to think about well, why? You know, what happened? Was it an intolerance issue, or was it some – or maybe I don’t have your history correct. Because really, these patients, particularly when they have not just diabetes but chronic kidney disease, they really have – I put them on a very strict LDL cholesterol target of less than 70, and so, therefore, you know, that is most of my patients I see in my clinical practice.
But what about triglycerides? So when you’ve had the patient stabilized on a statin and you know they’re taking it and you know they’re adhering and you see some LDL lowering, which is great, but that triglyceride level remains stubbornly above 150 mg/dL, those folks are at increased risk of cardiovascular events due to that high triglyceride level. And so the guidelines from the ACC/AHA recommend it’s time to think about using icosapent ethyl for those individuals. We’re going to get a lot more into icosapent ethyl soon.
So in terms of conditions, I’m not going to belabor everything on this slide, but know that when you see patients with type 2 diabetes, very frequently they will have elevated triglycerides as well. The things we can modify and we can make a difference in on this list, in terms of conditions: alcohol use. Alcohol use has increased during the pandemic, so there’s my second reference to the pandemic, and so that’s something we really want to be mindful to discuss with patients. Particularly when it’s in excess, triglycerides are going to go up. The other thing that I would mention would be hypothyroidism. When we don’t treat hypothyroidism adequately, triglyceride levels tend to go up.
In terms of medications, we can’t just take off all patients’ medications. Some of them are quite necessary, especially when we think about antiretroviral regimens. Although some drugs for HIV have more potential for causing metabolic disturbances to the lipid profile than others, so that’s something to think about in somebody who has HIV and perhaps multiple cardiovascular risk factors. But the ones I’ll call out on this list that you could change would be oral estrogens. I’m a big believer in treating menopause with estrogen when there are significant symptoms, when those symptoms are disturbing or disabling, because I think we undertreat those symptoms, unfortunately, particularly in the perimenopausal and early menopausal years. But I also want to get those medications, the estrogen, off as soon as the symptoms have abated and patients are feeling better, because for one fact, that’s going to improve their triglyceride levels. The other thing I’d be careful with is non-selective beta-blockers. Outside of patients who have anxiety, there’s just not a strong role for them. They’re really not preferred in terms of treating hypertension, so I try to stay away from those drugs, in part because of their negative effects on the lipid profile.
So second up, what’s up next in in terms of managements? Everybody’s favorite, it’s time to focus on lifestyle, diet, and exercise. And I usually like to recommend just starting with, I think, a pragmatic goal. 5% weight loss is a good pragmatic goal for many patients. Sometimes it’s even less than that. But I know that 5%, you start to have a difference in terms of disease markers and, you know, this last bullet point here is great: For every 5% to 10% decrease in weight, you get about a 20% lower triglyceride level. And in randomized trials, where patients are getting coached and they’re getting lots of follow-up and support, you can see pretty dramatic reductions in triglycerides related to changes in body weight, but also, you know, change in physical activity, changes in diet and, again, reducing alcohol is very important if that’s something your patients are drinking frequently.
So what about medical therapy? Of course, we’re going to talk about that too. So you really want to optimize statin therapy, and then the ezetimibe is something that has been proven to be effective, and this is our pathway. We’re really looking at LDL and lowering that major cardiovascular risk factor, and if necessary, a PCSK9 inhibitor, evolocumab or alirocumab, could be indicated as well. But for many patients, you still have this elevated triglyceride level. Now, there is a different pathway, as well, that’s espoused by major guidelines, and that would be to follow the triglycerides and try to lower that triglyceride level specifically with icosapent ethyl. And we’ll talk about “why icosapent ethyl?” quite a lot. But so this is something you want to bear in mind. So overall the theme here is don’t forget about triglycerides as an important cardiovascular risk factor, along with blood pressure, along with diabetes control, et cetera.
Now, some of these different adjuncts to statins have been proven to be successful. Ezetimibe has data from a randomized controlled trial with IMPROVE-IT. It was also, this year, demonstrated to be as effective in preventing cardiovascular events when combined with a moderate-intensity statin as a high-intensity statin alone. So ezetimibe has potentially some role. The PCSK9 inhibitors, we know they are very effective at lowering LDL-C, and they have also been associated with improvement in cardiovascular outcomes beyond the use of the statin, whereas fibrates and niacin just don’t have the data to support them in terms of cardiovascular risk. And we still see a lot of folks taking fibrates because of potential cardiovascular complications, especially with the publication of the PROMINENT study, which I will cover the results with you shortly. But it was really like an ideal population with type 2 diabetes and folks with high triglyceride levels, where it would seem like if any group would improve in terms of cardiovascular rates with a drug like pemafibrate at a good dose versus placebo, it was that group, and they didn’t. The trial was stopped early because of perceived futility of the active treatment, which is a shame, but they really kind of put the nail in the coffin when it came to the use of fibrates, and there really is no good evidence to use them for the prevention of cardiovascular disease overall.
Let’s look at fatty acids now. So, well, it’s all just fish oil, and so it’s got to be good for me, right? And so that may not be true, and actually, there’s even some evidence that some supplements could be potentially harmful. And so I think it’s important to separate out and spend a little time thinking about EPA versus DHA [docosahexaenoic acid]. There are different biological effects, and certainly, there are different outcomes in clinical trials.
We’ll start with the important stuff that actually matters to patients, which is the clinical trials. So you can see that when EPA has been mixed with DHA there have been a number of well-done studies that have looked at the use of EPA and DHA in terms of the risk of cardiovascular disease, and they generally have had no results; you can see. And again, you know, these trials go back over a decade. So there’s kind of a long history of futility in using mixed omega-3 fatty acids for the prevention of cardiovascular disease, except for this JELIS trial – J-E-L-I-S. Now, JELIS was the only positive trial in this list that when we look back on the history of these trials. And by the way, it was the only that included a pure EPA formulation in it.
Now EPA versus DHA, they look very similar; you can see they’re compared. EPA is on the top; DHA is on the bottom. This is a clever slide in that even small structural differences can have large biological differences because look at how close testosterone and estrogen are in terms of their biochemical structure. So always good to return to our biochemistry. Again, returning to clinical trials, when we separate out those EPA-only trials versus the DHA + EPA trials, you can see there’s a clear separation in benefit in terms of this forest plot – those blue dots with lines are the EPA-only trials – clearly favor all of these different cardiovascular outcomes compared with the combined fatty acid products. As we’ll get into, it’s not just about triglyceride lowering. Triglycerides are a good marker, and I definitely expect when patients start a drug like IPE, their triglycerides will come down, but it’s just like statins; there’s more to it than just their effects on the lipid profile itself. So it’s about membrane stability, it’s about reducing oxidation and inflammation, and so there’s several different effects of EPA that DHA doesn’t have, and that is probably somewhere in that mix of more salutary effects associated with EPA versus DHA and, on this table you can see, versus fibrates as well. That’s kind of the magic that EPA has that DHA and fibrates lack. So it’s not just about triglyceride lowering, as I’ll get into, it’s really about getting these other factors where, yeah, they address those multiple pathological factors and variables associated with the risk of cardiovascular disease.
This is data from REDUCE-IT. So this is a major trial looking at folks at elevated risk of cardiovascular disease on a statin where IPE or placebo mineral oil was added. And you can see that the rates – there was a good separation that, you know, you could really start to see the difference emerging even at 1 year in this cohort of patients, that the folks who took IPE were at a lower risk of cardiovascular events overall. And I’ll get a little bit more into these results in a second. But, again, it wasn’t just about triglyceride levels, because when we think of – remember the slide where I showed you how LDL was important, that the lower LDL you go, particularly in folks with a high risk of cardiovascular disease, the lower the risk of cardiovascular events. Well, here, you know, regardless of whether patients achieved a triglyceride level of 150 or more, or less than 150, they still have the cardiovascular benefit.
In the JELIS trial, referring back to that earlier trial which was done in Japan where they have a lot of great research looking at EPA overall. The idea here was to make it pragmatic. So we know statins are foundational therapy. We’re not replacing a statin with IPE; we’re adding onto it among folks who have high triglycerides. And this was a higher dose, too, of EPA, particularly pure EPA. You know, maybe previous trials had not necessarily dosed it correctly, so this was 4 g a day, so it’s 2 g twice daily and preferably taken with food. So that was the setup for the trial.
In terms of who were the patients in REDUCE-IT, they were at least 45 years old; they were treated with a statin. About 70% of folks had a prior history of cardiovascular disease or they had diabetes plus 1 risk factor. They had elevated triglycerides between 150 and 500 mg/dL, and they had an LDL level that was at likely to be near goal for them because it was at least less than 100. And you can see for the primary composite endpoint of the major adverse cardiovascular events, there was a relative risk reduction of 25% with a number needed to treat of 21. And when we looked just at cardiovascular death, MI, or stroke, a similar amount, 26.5% reduction with a number needed to treat of 28. So pretty remarkable results and really a well-done trial that argued strongly that icosapent ethyl will have real-world benefits for individuals who have elevated triglycerides, who have a high cardiovascular risk, and are treating with statins.
So another trial that’s come out fairly recently, published in 2020, was the STRENGTH trial. Well-done randomized trial taking 13,000 patients, and another trial that was stopped for futility after they got about 1,600 MACE endpoints. And this was using either corn oil as a placebo or a combined omega-3 fatty acid. So similarly to previous research, it was another trial that was a large-scale trial, a well-done trial that really didn’t demonstrate a difference with those mixed EPA/DHA fatty acids in terms of cardiovascular outcomes.
So let’s talk about pemafibrate in PROMINENT because this was a trial that was well designed. It was set up with a strong hypothesis based on the fact that folks who seemed to improve in terms of their cardiovascular risk with fibrates in the past were folks with type 2 diabetes, folks with high triglyceride levels, which is a really common thing we see in our clinical practices. So that’s who they aimed this trial at. So folks with type 2 diabetes. And you can see that two-thirds of them actually had a prior cardiovascular event. They all had triglyceride levels between 200 and 499, so elevated risk there as well. They are placed on pemafibrate twice daily or placebo and followed for major adverse cardiovascular events.
This is nice just because, well, gosh, was there a difference between these 2 major trials in terms of REDUCE-IT looking at icosapent ethyl, PROMINENT looking at pemafibrate? Were the profiles of patients different and that’s why there were different results? Because I think I already mentioned that PROMINENT yielded null results; it was stopped early. I don’t see a strong difference. You can look at these variables, but you know, there’s not really a strong difference in terms of the baseline characteristics of one cohort versus the other, but the results certainly were quite different in terms of the hazard ratios. None of them were significant when they looked at either composites or individual MACE outcomes. And overall mortality was similar as well. So really, like I said, this was a major trial because we have so much to do with our patients that, you know, we have multiple risk factors to take care of, multiple health issues to take care of. And so taking fibrates off the table, I think, is a good idea at this point, save for those individuals with a very elevated triglyceride levels even after they may be on a statin and they’ve tried lifestyle changes. That’s who a fibrate is for, more thinking about prevention of pancreatitis. But for the majority of my patients, where we really are thinking about cardiovascular protection, let’s use something like IPE when the triglyceride levels are high.
RESPECT-EPA is another study I will cover really briefly. This was done among folks with a low EPA-to-arachidonic-acid ratio who received statins. They all had coronary artery disease and had been on statins. And what this one showed is that using another purified EPA, that over time there was a reduction in terms of cardiovascular events, including cardiovascular death, and a secondary endpoint that was, you can read there, that is death, MI, unstable angina, or coronary revascularization. Again, there was a significant improvement over time.
And just thinking about some of these different trials looking at EPA versus, you know, that use different concentrations of EPA, JELIS and RESPECT-EPA were in Japanese populations, and not surprisingly, EPA concentrations at baseline were higher in that population. But even when you’re coming from a population that’s more mixed, including a lot of residents in North America, you can see that their EPA levels are lower, but there is a strengthening of the EPA effects, particularly with REDUCE-IT, right up to the levels that they achieved in either JELIS or RESPECT-EPA. So the EPA levels do increase even if they’re coming from a lower baseline.
So in terms of the bottom line for patients with elevated triglyceride and elevated risk of cardiovascular disease, it is drug. Icosapent ethyl stands out because of all that trial data I just cited to support that. Purified EPA really does make a difference, and it has some of the pharmacological qualities and molecular qualities that really help it succeed in terms of clinical trials. It’s not just that; it’s the dose as well. The dose is high, so using a sufficient quantity, 4 g per day, I think is really critical to making IPE work. And then with that in place, when you have the right patient, you have the right drug, and you have the right dose, it does make a difference in terms of cardiovascular health.
So overall, we can’t just focus on LDL. Again, statin drugs are foundational. Ezetimibe, PCSK9 inhibitors, they definitely have a role too. But so does IPE in particular. Why? Because it has the best clinical trial evidence. So again, looking at major guidelines based on trials like REDUCE-IT, if you have a patient with elevated cardiovascular risk, diabetes, or preexisting cardiovascular disease, they have a triglyceride level above 150 and they’re not responding to – particularly when they’re not responding to lifestyle interventions and/or removing some drugs that could be offensive, yeah, do think about icosapent ethyl. It can make a big difference and hopefully really prevent the next heart attack, stroke, or even death.
So with that, I’m really excited to hand off to Mary Katherine now, and she’s going to talk to you about the critical role for the pharmacist in lipid medication access and usage.
Dr. Cheeley:
For those of you just tuning in, you’re listening to CME on ReachMD. I’m Dr. Mary Katherine Cheeley, and here with me today is Dr. Chuck Vega. We’re discussing patient management and ASCVD risk reduction.
So let’s jump right in and talk about the role of a pharmacist in different cardiovascular care. There’s so many different hats that we wear as pharmacists; it’s not just patient-specific and it’s not just facility-specific. But overall, we have such a role to play in all 3 different aspects, including global services. It’s important that the patient in front of us is always the number one thing that we’re thinking about, but when we talk about facility-specific with guidelines and different order sets, ways that we can help our physician partners and other prescribing providers make the right clinical decision for patients. And then, in addition to that, we have global services with not just public health initiatives, but involvement in different society guidelines, which we’ll talk about a little bit more.
There’s so many different ways to approach cardiovascular risk reduction, and I’ve been in practice 13 years at this point, and I promise you there has been so many advances in an area that I wasn’t sure we could do much more in. So it’s really exciting, all of the things that are coming down the line for cardiovascular care. But more than that, it’s important to understand that most of our therapies for cardiovascular risk reduction are on the backbone of maximally tolerated statin therapy.
I would be remiss if I did not talk about the different intensities of statins, so remember high-intensity atorvastatin 40 and 80 and rosuvastatin 20 to 40 are what our goal is to get patients on. But it’s not just the dose of the statin that matters; it’s also important that we think about getting patients to goals, and with getting patients to different therapeutic objectives.
It’s well known that not all patients will tolerate statins in the same way, and it’s also well known that not everyone will have the same LDL-C response. So in the JUPITER study you can see that most patients, even though they were receiving rosuvastatin 20 mg, some patients didn’t have the anticipated about 50% reduction in LDL cholesterol. They didn’t have the same reduction, even though they were getting the same dose. But we do know that every time we lower LDL cholesterol by 40 mg/dL, we have about a 25% reduction in hard major adverse cardiovascular events, of cardiovascular death, MI, and stroke. This has been seen all throughout major clinical trials for lipid lowering. So while we may not get the same reduction in LDL cholesterol for patients, even though they’re getting the same dose, we know that if we achieve the same LDL reduction, no matter how we get there, it’s important to understand and remember that we will still have that reduction in hard cardiovascular endpoints. And that’s been seen with multiple different adjuncts: ezetimibe, PCSK9 monoclonal antibodies, and even more recently, the bempedoic acid trial of CLEAR Outcomes.
What we haven’t seen is positive studies with fibrates and niacin. So current guidelines and current guidance tell us that combination statin fibrate, it’s not been shown to improve ASCVD outcomes, and it’s not really recommended. Same with statin and niacin. However, when you have a patient specifically with diabetes and ASVCD, if the LDL cholesterol is great than 70, and in most cases now greater than 55, it’s important that we think about additional LDL-lowering therapy with either ezetimibe, a PCSK9 monoclonal antibody – which when I’m saying those, I mean alirocumab or evolocumab; those are the 2 that have outcome studies – and now additionally, bempedoic acid.
But we also know that statins are wonderful drugs, and most often they’re really well tolerated, but they’re not that easy for some patients to take. There is a very real effect called the nocebo effect that patients experience. So yes, we know that statins are great and three-quarters of the general population can certainly take a statin, but we also know that of the millions of patients that take these drugs, 10% to 20% of them, which is a decent amount, have some type of reported statin intolerance. So it’s important that we as pharmacists in that first line of providers that patients will come and talk to, or providers who are doing MTM [medication therapy management] or adherence check-ins on our patients with our targeted interventions, with our TIPs [Targeted Intervention Programs], that we can notice this probably before the provider will notice it. We’re going to be able to see this patient’s not picking up their statin on time, or hey, they’re kind of delayed, and I have to call them every month to remind them to take their statin. So this is where we can have such a huge impact.
In 2022, the National Lipid Association [NLA] actually updated the definition of statin intolerance to be defined as 1 or more adverse effect associated with statin therapy, which then resolves or improves with dose reduction or discontinuation. The new part of the definition is that it can be classified as complete or partial intolerance, and it’s the inability to tolerate the dose necessary to achieve patient-specific therapeutic outcomes.
So a large portion of patients tend to discontinue their statin therapy within 1 to 2 years, and that’s heartbreaking to me. These drugs are really, really well tolerated, and they’re really easy to take – it’s one pill once a day – but we still have a huge proportion of patients that are not on their drug after having an actual event. So the National Lipid Association also, in 2019, published the STATE survey, which is the STatin Adverse Treatment Experience survey. So we looked at 1,500 patients who had a statin intolerance, self-reported, within the last 6 months, and you can see that even those patients who stopped their statin within the last 6 months were still able to tolerate something. So some lowered their dose, some were switched to a different statin, but you can also see that it’s really important that something is tolerable for patients. Now it may be that partial intolerance, but it’s important that we don’t kind of just give up after 1 drug and that we engage our prescribing and physician partners to talk about the different strategies, lowering the dose, switching from something that’s lipophilic to something that’s hydrophilic, or working on alternate-day dosing. And all of this is laid out, also, in that new statin intolerance document and definition. There’s also a statin-associated muscle symptoms paper that the NLA just published as well. So these are great strategies.
But even with all of that, it’s really important to understand that there’s still this gap for our patients. LDL-C reduction is wonderful, and it’s something that we need to make sure that we are working towards with our patients, but there’s still a gap for patients who are high risk with stable ASCVD or have diabetes and they can’t get to that non HDL-C goal either, and that’s where icosapent ethyl comes into the picture.
So in 2019 the package labeling was updated for icosapent ethyl to show ASCVD risk reduction for patients who have MI, stroke, coronary revascularization, and unstable angina, and they have an elevated triglyceride which was greater than 150 mg/dL. So now we have not just the LDL-lowering way of reducing cardiovascular risk reduction, but also the total atherogenic lipoprotein profile for patients when looking at their non HDL or having elevated triglycerides for patients. And there’s more than 30 different medical societies that will back this up and have now adopted it into their standards of care or their guideline documents.
But I want to caution you as pharmacists. So a lot of us have worked retail or a lot of us are kind of the first line of education for our patients. Not all EPA and DHA products are the same. So just like Dr. Vega talked about before, you have dietary supplements, you have the combination prescription product, which you can see are a mixture of DHA and EPA, and I know he’s talked about the different biological effects of EPA and DHA. So it’s important to kind of understand when your patient comes to you with a bottle of fish oil that’s over the counter or is a dietary supplement, you understand that it is not the same as what they’re getting from the prescription side and that even the prescription omega-3 fatty acids are not the same as icosapent ethyl or a pure EPA-only product.
Not only that, but our dietary supplements are not well regulated. So we used to joke in pharmacy school that you could just put grass in your bathtub and kind of stuff it in a capsule and call it a dietary supplement, and you would be done. Because they’re just not regulated the same way that our drugs are. So yes, we do have USP [US Pharmacopeia], and that is a wonderful resource for us to know that at least there’s good manufacturing practices, but it doesn’t mean that everything has a USP sticker on it, and it doesn’t mean that just because they’re manufactured well that they don’t have other harmful ingredients in them as well.
So I think a picture is worth a thousand words, and you can actually see in the right-hand side of this picture the dietary supplement which looks milky and fatty and kind of like the bacon tray after you pull the bacon out of the microwave or out of the oven and let it sit for a little bit. That’s what that looks like to me, not that I eat bacon. We don’t eat bacon; it’s fine. But you can see the other one with the prescription omega-3 is much clearer; it’s much more pure. So it’s important for our patients to understand that while, yes, dietary supplements may say that they have EPA and DHA, number one, you remember that it’s a different component of it, but also, these actually also can be harmful. So saturated fats, we know, lead to an increased risk of cardiovascular disease, and so patients may think that they’re doing something right for themselves, but unfortunately, if they’re just adding 4 to 8 capsules of saturated fat into their diet every day by doing something that they think is healthy, it may not be.
So let’s spend a little bit of time talking about the different warnings and precautions for icosapent ethyl because I get asked about these a lot. So atrial fibrillation was definitely seen in the original studies for icosapent ethyl, but it was a very small proportion of patients, and it was in patients who already had a history of A-fib or A-flutter. So this wasn’t new-onset A-fib and A-flutter, but it was seen in those patients. There is a very small, minute potential for allergic reactions; however, I will say it’s an extremely pure version of icosapent ethyl, and so patients who have a shellfish allergy, generally, I do a little bit more investigation with the patient. So is your shellfish allergy, oh, my goodness, you just look at a shrimp and you’re in the hospital – okay maybe I wouldn’t do that. Or is it, hey, I eat an entire plate of shrimp or crawfish or whatever it is, and then you know, the next day I might be a little itchy. Those are 2 different pictures in my mind, and so it’s important to kind of talk to your patient about that. But more than likely, because it's so highly purified, a lot of these patients, unless they have a very severe allergy, will do fine. It’s just important to give them that anticipatory guidance as a pharmacist: hey, if you notice X, Y, and Z, do not pass go, do not collect $200, go straight to the ER if there’s something that you’re concerned about.
The other thing I want to talk about is increased risk of bleeding. So it is known that omega-3 are antithrombotic and therefore can cause a little bit of bleeding. It’s well known with icosapent ethyl and also the prescription omega-3 fatty acid products. So again, is this a patient who is on a full-dose DOAC [direct oral anticoagulants] and aspirin and clopidogrel? That’s a totally different picture to me than someone who’s on warfarin and their INR [international normalized ratio] is consistently in range and they’ve been in range for 10 or 15 years. So it’s important that we also give that anticipatory guidance to patients. Hey, if you are on this and this is new to you and everything else has been stable, these are the things that you need to look out for.
Overall, I will say that prescription omega-3 fatty acid products are really well tolerated, and the AHA Science Advisory Committee also went through all of these different aspects that we just talked about so that we can make sure that we’re giving our patients safe medications, safe different anticipatory guidance so that we make sure that we’re keeping our patients as safe as we can.
So the biggest thing I can talk about from the provider side of it and being in a lipid clinic is making sure that we monitor the response to all of our drug therapy that we give our patients – not just icosapent ethyl, but also making sure with our monoclonal antibodies, making sure with our statins. Patients really like to know where they’re at. They really like to know how much percent lowering, where did I come from, so what did my LDL start at and now what is it later? They love to know that they’re getting somewhere. We as human beings like to know that we’re achieving something. So it’s really important in my world to make sure that we are monitoring a response to these therapies. But in addition to that, we also know that lifestyle modifications are really hard, and so it’s important that, yes, drugs are super important, but also making sure that we’re keeping an eye on those lifestyle changes that our patients are making, encouraging them to have a healthy diet, encouraging them to have a healthy lifestyle. And then if we find a patient who tends to have maybe some genetic reason for having an elevated risk that we cascade screen and let them know to get their family screened, their kids, their grandkids.
So if I leave you with anything about this, I would love to make sure that you remember that dietary supplements are not all equal. They’re not the same. Prescription omega-3 products are purified. They are much cleaner, much safer for our patients. But even more than that, a mixed DHA/EPA is also not equal to an EPA-only product with icosapent ethyl. The other thing that I think providers and patients always forget is that it’s 2 g twice a day. So preferably with a meal, with breakfast and with supper, but 2 g twice a day is the dose that has been studied. That is hard for patients to swallow, both figuratively and literally. But it’s important that we as pharmacists do that counseling, again, when you’re doing your TIPs, when you’re doing your MTMs, making sure that you are educating your patient – it’s not 1 pill twice a day; it’s 2 capsules twice a day – so that they’re getting all of the benefit that they can. And then also make sure that you’re talking to your patients about not only the safety concerns, but all of the amazing things that are happening in the lipid space. Because if our patients are excited about where we’re going with our medical knowledge and what we can do for them to reduce their risk, then they’re more likely to be engaged in the process, and we can do a better job of taking care of them.
So now that we’ve talked about the evidence and we’ve talked about all the different things that we need to talk to our patients about in our counseling, I want to go through a couple of cases. So, Chuck, why don’t you take us through our first one?
Dr. Vega:
I’ve got a 61-year-old woman to tell you about. She had inferior wall MI 9 months ago, unfortunately. She’s a smoker, hypertension, she’s on an angiotensin receptor blocker, fairly sedentary. We see blood pressure is fairly well controlled, 126/78, but her BMI is 31; A1c is 6.3%. She has prediabetes. She was not on a statin prior to her MI. Her LDL was 144 at that time, triglycerides 167, total cholesterol 217. Now, she was started on atorvastatin 80 mg, great idea. But she stopped it due to severe bilateral thigh pain after 1 month. Then she tried rosuvastatin 10 mg once a day and then it was once a week, and then she went on to pravastatin 40 mg every other day. Mary Katherine, she’s definitely following the plan for statin intolerance that you espoused, but just not getting there. She was able to tolerate ezetimibe, so that’s what she’s taking now, and on ezetimibe her LDL cholesterol’s still 120.
So she was started on evolocumab. She’s using that twice a month. Importantly, she really started picking it up in terms of activity, walking more. She lost 8 pounds; she stopped smoking, which is the most important factor in terms of her cardiovascular risk. And her repeat labs show the LDL did come down to 73, HDL is now 43, triglycerides are 151, and total cholesterol is at 146. You know, so she’s doing some lifestyle changes now and her LDL looks a lot better.
What do you think, Mary Katherine? Where do you want to go with this patient?
Dr. Cheeley:
She is doing everything right. So she’s on a monoclonal antibody, which I think is great for her. I love that she is on and tolerating her ezetimibe. I would continue to push lifestyle in her. So I think it’s really important that, like you talked about in the REDUCE-IT trial, while the package labeling is 150 mg/dL for triglycerides, they did see benefit all the way down well below 100. And so it’s something that we can think about in her is, is she willing to take an additional 4 capsules a day? Is she willing to kind of go down that road? What are her goals? I love that you talked about shared decision-making with this patient because it’s not just treating a number; it’s really making sure that we’re looking at the whole patient. I love that she stopped smoking. Can we, like, make her the poster child for all of our patients?
Dr. Vega:
I agree. I’m not sure I want to stop her momentum right now. I always try to see the trajectory. If she’s really excited about the fact that she made the positive changes and I can feel that and she wants to continue them, “What else can I do?” and, you know I’m sensing that hunger, yeah, I’m going to let this ride. I am thinking about IPE in the back of my head, as you mentioned. It could a really good option for her, but I know if she continues to lose weight, for example, you know, those triglyceride levels will keep falling, as well, and her overall cardiovascular risk will come down. So I think that she’s in a much better place, it’s exciting, and we will still think about IPE in her future. That’s what continuity is for.
Dr. Cheeley:
That’s right.
Dr. Vega:
So we’re 1 for 1; we’re on the same page. Do you want to talk about another patient?
Dr. Cheeley:
I do.
Dr. Vega:
Awesome. All right, so this one is a little different. So 61-year-old woman. History of coronary bypass graft in 2003. She has dyslipidemia, hypertension, type 2 diabetes, and obesity. We know that she has plaques, confirmed subsequently on a coronary CT [computerized tomography]. She underwent a stent placement in her femoral arteries, so she has peripheral artery disease as well. And then she was experiencing some angina with exertion, so she is here to follow up her nuclear stress test. So sounds like, you know, she is still somebody with a long history of coronary artery disease and now with ongoing risk factors and ongoing symptoms as well.
So how are we doing in terms of our med management? I automatically get my little checklist out and are we able to treat her appropriately given that history? She is on an antihypertensive combination olmesartan and chlorthalidone, amlodipine, carvedilol, rosuvastatin – okay, ding ding – ezetimibe 10 mg – ding ding – clopidogrel, yes; metformin, yes; and semaglutide. Okay, so not too shabby with regards to her regimen so far.
Mary Katherine, do you have any comments when you hear that medication list?
Dr. Cheeley:
I have so many thoughts about Miss Catherine. While she’s on some of the right medicines, I think her rosuvastatin certainly could be optimized. But remember, when we double the dose of a statin, we’re only going to get an additional 6% lowering, and right now her LDL cholesterol is sitting at 82. And her triglycerides are far too high, assuming these are fasting labs, which we always want to make sure when our patients have triglyceride disorders, we’re getting fasting labs. So I’m not sure that really pushing the dose of her statin is something that I would pursue at this point; I think she’s got to have additional therapy. And because she has ASCVD and multiple vascular beds, I really desperately want her LDL cholesterol to be less than 55. I think that’s one of the great things that are listed in both the ADA [American Diabetes Association] and the new consensus statement, that as we know that patients have progressive disease – she had a CABG [coronary artery bypass grafting]; we put new vessels attached to her heart and she still is having progressive plaque placement. So I think it’s important that we continue to drive her LDL cholesterol down, but also keeping in mind that her triglycerides are another part of the picture. I don’t see an A1c in her. That’s something that I would also want to know. Do we continue to push her semaglutide? But something that I think is really important on these labs, that you also mentioned when you were talking, is her Lp(a); that is high.
Dr. Vega:
Right.
Dr. Cheeley:
Her Lp(a) is 118 nmol, and so I think that we really need to get her on some therapy that will decrease that Lp(a) as much as we can, and for me, that’s a PCSK9 monoclonal antibody. And continue to work with her on her lifestyle in terms of helping her glucose come down, being more physically active. But with that Lp(a) and that LDL cholesterol, I’ve really got to focus on that first.
Dr. Vega:
Well, I actually didn’t mention her labs, but you were clearly enthusiastic about looking into them and being very proactive in terms of knocking down her risk. But you’re absolutely right. You know, it’s funny because I really appreciate the perspective. I would probably start with, gosh, are you taking your rosuvastatin, ezetimibe regularly? Because, you know, when you see an LDL-C on that combination and it’s 82, many times, it just says, eh, I’m taking it. Yeah, I see you taking it twice a week, but it turns out she has been adherent and then, yeah, therefore absolutely right when you factor in the Lp(a) elevation, PCSK9 in her makes a lot of sense, and actually that exactly is what was added. So you’re prescient and, you know, you’re really all over it. Now turns out that moving forward, her angina is improving, but we’re still concerned about her triglyceride levels. So because even when we add on a PCSK9 inhibitor, we can’t necessarily expect the triglyceride levels to improve that much. So what do you think about her as a potential candidate for IPE?
Dr. Cheeley:
I think she’s a great candidate for it if it’s something that she’s willing to do. I do think that it could help her in multiple different ways. So like I mentioned, she has disease in multiple different vascular beds, and so if we’re adding it, that helps us not only with lowering her cardiovascular risk, but also, like you mentioned, thrombotic-wise. So she is on clopidogrel. I assume she’s probably taking an aspirin as well. We need to think about that and counsel her on those points. But remember, also, one thing I want to point out, because you mentioned it with your rosuvastatin and ezetimibe, when you have an elevated Lp(a), you will not have the same anticipated response of LDL cholesterol reduction. So I think that’s really important when we as providers are looking at the labs and you’re not seeing that anticipated response, yes, the first thing I always ask is, are you actually taking it? Do you actually swallow those tablets? But if the answer is yes and I can prove that by making sure that they’re adherent to their therapy, filling things on time, again, if I’m the MTM pharmacist doing a TIP on this patient, it’s going to be a little bit different of a conversation than if I’m in the office with them. But we don’t always see the anticipated response, and so it’s really important that we’re hitting this from multiple different avenues of the LDL reduction, so adding on evolocumab or alirocumab, whichever one is covered by her insurance, and then if we add on IPE, then that’s just an extra layer of added benefit that we can get for her to reduce her cardiovascular risk.
Dr. Vega:
Yeah. I agree. And it’s a question of whether she will be able to take it, as you mentioned with shared decision-making. You know, a little bit concerned, with an antiplatelet agent on board, about her risk of bleeding, but I didn’t see any bleeding history there. You can always use a calculator like HAS-BLED, too, which is a validated calculator. We’re thinking about at least anticoagulant-related bleeding. So therefore, I think she’s a great candidate, and if she’s willing to move forward and go with it, especially considering she has ongoing symptoms, you know, gosh, risk reduction – this is an all-hands-on-deck case, because really, she has not only the risk factors, but she has ongoing disease with ongoing symptoms. Very, very concerning.
Dr. Cheeley:
Unfortunately, that’s all the time we have today. So I want to thank you, our audience, for listening in and thank you so much to Dr. Chuck Vega for joining me in sharing all of your valuable insights. It was so great to speak with you today.
Announcer:
You’ve been listening to a replay of a live broadcast discussing a collaborative approach to reducing ASCVD event burden in your high-risk statin-treated patients. This activity was provided by Medtelligence and is supported by an independent educational grant from Amarin Pharma, Inc.
To receive your free CE credit or to download this activity, go to ReachMD.com/CME. This is CME on ReachMD. Be Part of the Knowledge.
Disclosure of Conflicts of Interest
In accordance with the ACCME Standards for Integrity and Independence, Global Learning Collaborative (GLC) requires that individuals in a position to control the content of an educational activity disclose all relevant financial relationships with any ineligible company. GLC mitigates all conflicts of interest to ensure independence, objectivity, balance, and scientific rigor in all its educational programs.
Host:
Mary Katherine Cheeley, PharmD, BCPS, CLS, FNLA
Executive Director, Ambulatory Pharmacy Services
Grady Health System
Atlanta, GAConsulting Fees: Novartis Pharmaceuticals
Faculty:
Charles P. Vega, MD
Clinical Professor, Family Medicine
University of California, Irvine School of Medicine
Santa Ana, CAConsulting Fees: Boehringer Ingelheim and GlaxoSmithKline
Reviewers/Content Planners/Authors:
- Jennifer Brutsche has nothing to disclose.
- Cindy Davidson has nothing to disclose.
- Howard Green has nothing to disclose.
- Andrea Mathis has nothing to disclose.
- Tim Person has nothing to disclose.
- Mario Trucillo, PhD, MS, has nothing to disclose.
Learning Objectives
After participating in this educational activity, participants should be better able to:
- Outline the biologic effects of omega-3 fatty acids and their mechanisms of action, differentiating icosapent ethyl (IPE) from other agents
- Engage with physicians to interpret and relate recent clinical trial evidence regarding eicosapentaenoic acid (EPA) and the clinical implications for patients
- Distinguish the use of IPE in the management of ASCVD and define the shortfalls of dietary supplements
Target Audience
This activity is designed to meet the educational needs of pharmacists and managed care healthcare professionals.
Accreditation and Credit Designation Statements

In support of improving patient care, Global Learning Collaborative (GLC) is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC) to provide continuing education for the healthcare team.
Global Learning Collaborative (GLC) designates this live activity for a maximum of 1.0 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Global Learning Collaborative (GLC) designates this activity for 1.0 nursing contact hour. Nurses should claim only the credit commensurate with the extent of their participation in the activity.

Global Learning Collaborative (GLC) has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 1.0 AAPA Category 1 CME credit. PAs should claim only the credit commensurate with the extent of their participation in the activity.

Global Learning Collaborative (GLC) designates this activity for 1.0 contact hour/0.1 CEUs of pharmacy contact hours.1
The Universal Activity Number for this program is JA0006235-0000-23-084-H01-P . This learning activity is live. Your CE credits will be electronically submitted to the NABP upon successful completion of the activity. Pharmacists with questions can contact NABP customer service (custserv@nabp.net).Provider(s)/Educational Partner(s)

Our ultimate goal is to improve the care being delivered to patients, and our high-quality, evidence-based CME initiatives reflect our dedication to the creation and execution of excellence and are the product of shared research, knowledge, and clinical practice skills across the healthcare continuum.
Commercial Support
This activity is supported by an independent educational grant from Amarin Pharma, Inc.
Disclaimer
The views and opinions expressed in this educational activity are those of the faculty and do not necessarily represent the views of GLC and Medtelligence. This presentation is not intended to define an exclusive course of patient management; the participant should use his/her clinical judgment, knowledge, experience, and diagnostic skills in applying or adopting for professional use any of the information provided herein. Any procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this activity should not be used by clinicians without evaluation of their patients’ conditions and possible contraindications or dangers in use, review of any applicable manufacturer’s product information, and comparison with recommendations of other authorities. Links to other sites may be provided as additional sources of information. Once you elect to access a site outside of Medtelligence you are subject to the terms and conditions of use, including copyright and licensing restriction, of that site.
Reproduction Prohibited
Reproduction of this material is not permitted without written permission from the copyright owner.System Requirements
- Supported Browsers (2 most recent versions):
- Google Chrome for Windows, Mac OS, iOS, and Android
- Apple Safari for Mac OS and iOS
- Mozilla Firefox for Windows, Mac OS, iOS, and Android
- Microsoft Edge for Windows
- Recommended Internet Speed: 5Mbps+
Publication Dates
Release Date:
Expiration Date:
Related
Mastering the Management of ASCVD Risk!
Show more
Recommended
Advancing IgAN Care: Expert Strategies for Transformative Patient Outcomes
Advancing IgAN Care: Expert Strategies for Transformative Patient Outcomes
CME/CEAdvancing IgAN Care: Expert Strategies for Transformative Patient Outcomes
0.25 credits0.25 creditsImplementing a Successful Barostim Program in the Clinic: Best Practices and Real World Experience
Implementing a Successful Barostim Program in the Clinic: Best Practices and Real World Experience
CME/CEImplementing a Successful Barostim Program in the Clinic: Best Practices and Real World Experience
My Patient's At 'Low Risk' for Clinically Significant Fibrosis: What Should I Do Now?
My Patient's At 'Low Risk' for Clinically Significant Fibrosis: What Should I Do Now?
MinuteCE®My Patient's At 'Low Risk' for Clinically Significant Fibrosis: What Should I Do Now?
1.00 program credit1.00 program creditNoninvasive Tests for Clinically Significant Fibrosis: That's The Hepatologist's Job, Right?
Noninvasive Tests for Clinically Significant Fibrosis: That's The Hepatologist's Job, Right?
MinuteCE®Noninvasive Tests for Clinically Significant Fibrosis: That's The Hepatologist's Job, Right?
1.00 program credit1.00 program credit












Facebook Comments